content body
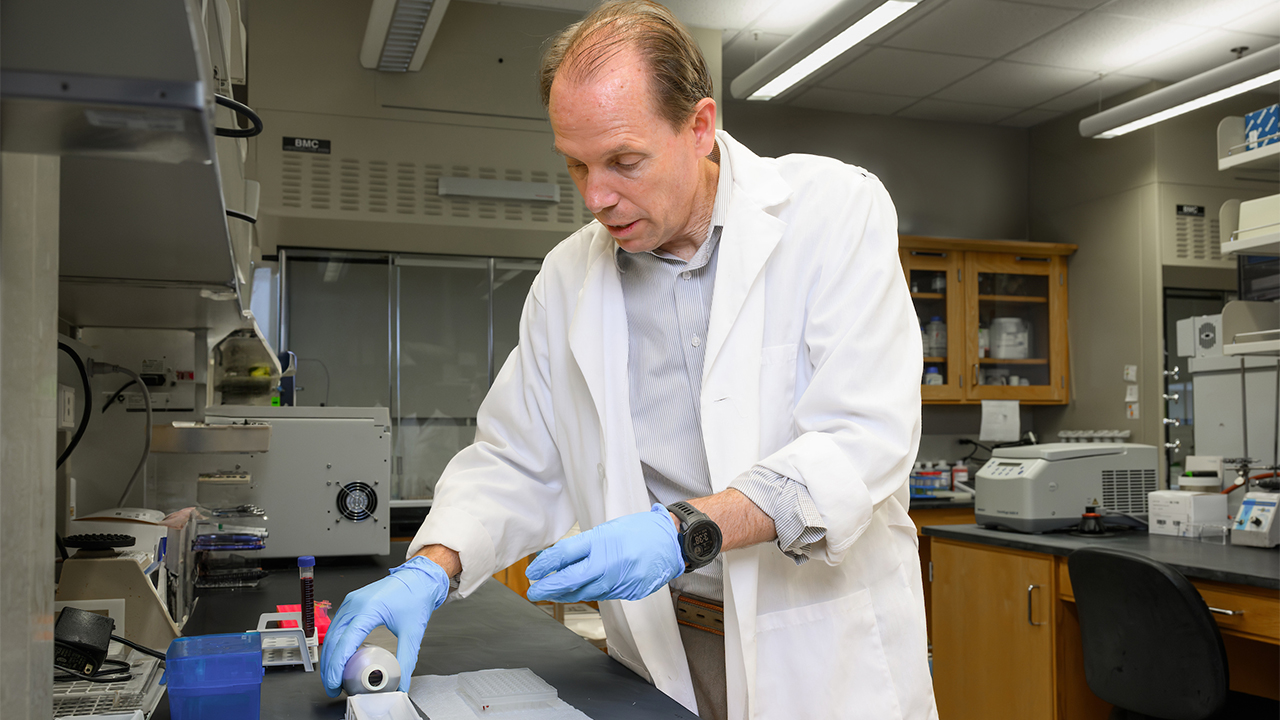
Professor Mike Greene has healthy living on his mind.
By day, he studies obesity’s role in chronic diseases in his laboratory within Auburn’s College of Human Sciences. Over the summer, Greene leads a study abroad program where a handful of lucky Auburn students experience the Mediterranean lifestyle in action. Closer to home, Greene may be found trail running, playing soccer, walking his dog in the Donald E. Davis Arboretum or baking a pizza in his backyard oven.
“For me, science and my personal interests are integrated,” Greene said. “I’m interested in both understanding the processes occurring within our bodies and taking a step back and thinking about our overall health and well-being.”
This synergy between Greene’s lifestyle and scientific pursuits works for him — and has proven fruitful in generating research funding.
Among his grants, Greene is principal investigator on an Alabama Agricultural Experiment Station USDA AIR grant and co-principal investigator with Elizabeth Lipke, the George E. & Dorothy Stafford Uthlaut Endowed Professor within the Samuel Ginn College of Engineering, on a R01 research award from the National Institutes of Health (NIH) for almost $2.5 million.
Greene’s recent grants are broadly focused on better understanding the connection between colon cancer and obesity.
“The association between colon cancer and obesity is pretty rock solid,” Greene said. “But now, we’re getting into the question: what is obesity doing to make cancers more dangerous?”
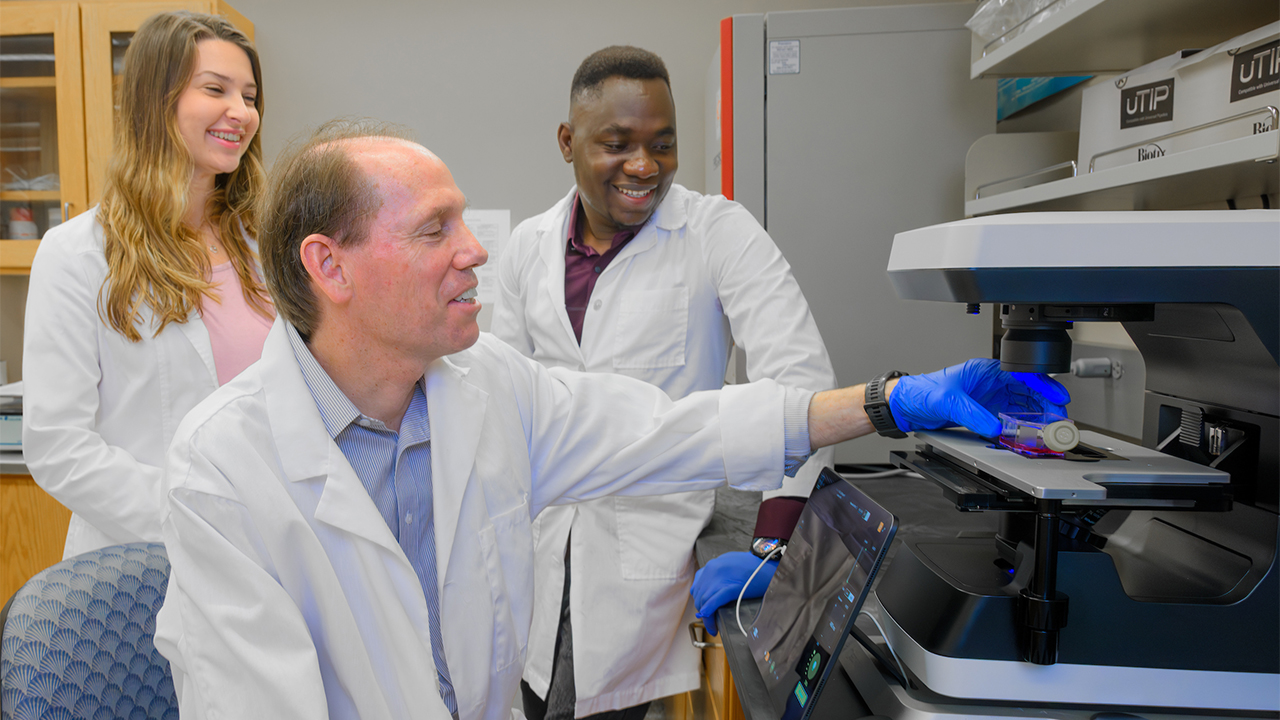
Greene and two of his doctoral students, Kathryn Edmondson (left) and Ifeoluwa Odeniyi (right) image live and dead cells.
Parsing the pathway between obesity, colon cancer
Greene said many Americans may be surprised to discover that being obese is associated with colon cancer — a relevant connection for many Americans.
Across the U.S., colon cancer is the second-deadliest cancer. The American Cancer Society estimates more than 100,000 people will be diagnosed with colon cancer in 2024. In Alabama alone, experts estimate that over half of the population will be obese by 2030. Greene’s goal is to help unravel how obesity and colon cancer are linked by studying the pathways that go awry within the human body.
“We have normal processes that occur in the body, and some of those go out of whack and that becomes pathological,” Greene said. “It’s this pathophysiology that I find very interesting.”
By studying the pathophysiology surrounding obesity and colon cancer, Greene and his colleagues found a high-fat diet sparks faster and larger tumor growth. They also discovered some differences in colon cancer types can be linked to obesity’s impact on gene expression by analyzing patients’ tumors. Greene and his colleagues published these findings in Nutrition Research and PLOS One, respectively.
“We’re still trying to tease out what is driving some of this dynamic,” he said. “One hypothesis is that insulin resistance is linked to inflammation, and we think that inflammation link is really driving colon cancer.”
To further explore the connection between colon cancer and obesity, Greene is collaborating with Lipke in their NIH-R01 research award. They are using patients’ tumor samples, known as patient derived xenografts, to create a 3D model of the cancer’s environment at the tissue level outside the body, or in vitro. Lipke brings expertise in creating these 3D models.
“Together with Dr. Greene, we are building 3D cell culture models of patient colorectal cancer and comparing them to his animal models,” Lipke said. “This highly synergistic collaboration enables our joint team to investigate obesity-related mechanisms driving cancer progression and test more parameters than is possible in animals alone.”
As part of their collaborative research, the scientists are particularly interested in gleaning insight about how colon cancer may vary among individuals. Experts already have discovered that colon cancer comes in a variety of different types, known as molecular subtypes.
“Cancer drugs don’t always work for everybody,” Greene said. “The question is, ‘why don’t they work?’ Well, there are lots of reasons why. But one is that some people’s tumors are just different from other people’s tumors.”
By recreating the tumor’s environment outside the body at the tissue level, the scientists can then test how the tumor responds to different drugs in a controlled setting. They can also better examine how obesity is impacting the tumor.
“If we can identify it and try to narrow down what’s effective, we could be moving toward a more personalized approach to cancer treatment,” Greene said.

Greene and his wife Paula Greene like to eat fresh produce from their garden. Photo credit: Molly Bartels
Meaningful summers in the Mediterranean
Long-term, Greene’s goal is for this collaborative research to improve cancer treatments. But that doesn’t stop him from exploring approaches to encourage healthy lifestyles now.
He also happens to love Italy.
“I traveled in Italy and really loved the food,” he said. “I loved everything about the whole lifestyle.”
A key aspect of this lifestyle is eating meals that are heavy in vegetables, fish, with healthy fats, such as extra virgin olive oil, and limited red meats, which is known as the Mediterranean diet in the States. Greene said he’s intrigued by more than just the foods one puts in their body.
“When you sit around for a meal for two hours, you’re not just eating, you’re talking and enjoying the company with other people,” he said. “It’s the social experience that’s a huge part of it.”
For the past six summers, Greene has given students a taste of the Mediterranean by bringing them on a three-week study abroad program to a variety of locations, including Greece and Italy. A day-in-the-life look at the study abroad program may have college-aged students — and many of their parents — feeling jealous.
“We could go visit an olive mill, learn about how to taste olive oil. And then in the afternoon, we could go swim in the Mediterranean,” Greene said. “Then, in the evening, we’re going to have a long dinner together.”
This study abroad program has sparked some students’ interest in embracing a healthy lifestyle or changing their major to nutrition. For Greene, the trip initiated new research ideas related to the Mediterranean diet. For example, he found that nutrition majors and people who regularly go to the farmer’s market are more likely to stick with the Mediterranean meal plan.
“The Mediterranean diet work is integrated into a lot of the things that I do, and it’s an important part of who I am,” he said.
Greene’s career path may be unconventional for a basic scientist — many researchers prefer to spend all of their time in the laboratory — but Greene says he’s grateful to have had this opportunity to carve out a unique career path.
“I’m very fortunate to be in the Department of Nutritional Sciences — the opportunity to do this study abroad was something that I never thought of,” he said. “This experience is something that I’ll cherish forever.”
Learn more about the three-week Mediterranean Diet study abroad program.
Click here.